Breast Procedures
What is Breast Reconstruction?
.jpg)
The goal of breast reconstruction is to restore one or both breasts to near normal shape, appearance, symmetry, and size following mastectomy, lumpectomy, or other trauma. Breast reconstruction often involves several procedures performed in stages and can either begin at the time of mastectomy or be delayed until a later date.
Breast reconstruction generally falls into two categories: implant based reconstruction or flap reconstruction. Implant reconstruction relies on breast implants to help form a new breast mound. Flap reconstruction uses the patient’s own tissue from another part of the body to form a new breast. There are a number of factors that should be taken into consideration when choosing which option is best:
- Type of mastectomy
- Cancer treatments
- Patient’s body type
Is it Right for Me?
Breast reconstruction is a highly individualized procedure. You should do it for yourself, not to fulfill someone else’s desires or to try to fit any sort of ideal image. Breast reconstruction is a good option for you if:
- You are able to cope well with your diagnosis and treatment
- You do not have additional medical conditions or other illnesses that may impair healing
- You have a positive outlook and realistic goals for restoring your breast and body image
Although breast reconstruction can rebuild your breast, the results are highly variable:
- A reconstructed breast will not have the same sensation or feel as the breast it replaces.
- Visible incision lines will always be present on the breast, whether from reconstruction or mastectomy.
- Certain surgical techniques will leave incision lines at the donor site, commonly located in less exposed areas of the body such as the back, abdomen or buttocks.
A note about symmetry: If only one breast is affected, it alone may be reconstructed. In addition, a breast lift, breast reduction or breast augmentation may be recommended for the opposite breast to improve symmetry of the size and position of both breasts.
Consultation and Preparing for Surgery
During your consultation be prepared to discuss:
- Your surgical goals
- Medical conditions, drug allergies, and medical treatments
- Current medications, vitamins, herbal supplements, alcohol, tobacco, and drug use
- Previous surgeries
Your surgeon will also:
- Evaluate your general health status and any pre-existing health conditions or risk factors
- Examine your breasts and take measurements of their size and shape, skin quality, and placement of nipples and areolae
- Take photographs
- Discuss your options and recommend a course of treatment
- Discuss likely outcomes of breast reconstruction and any risks or potential complications
Prior to surgery, you may be asked to:
- Get lab testing or a medical evaluation
- Take certain medications or adjust your current medications
- Stop smoking
- Avoid taking aspirin, anti-inflammatory drugs, and herbal supplements as they can increase bleeding
Breast reconstruction surgery is typically performed in a hospital setting, may include a short hospital stay, and will likely use general anesthesia. Some follow-up procedures may be performed on an outpatient basis, and local anesthesia with sedation may be used. These decisions will be based on the requirements of your specific procedure and in consideration of your preferences and your doctor’s best judgment.
Be sure to ask your plastic surgeon questions. It’s very important to understand all aspects of your breast reconstruction. It’s natural to feel some anxiety, whether it’s excitement for your anticipated new look or a bit of preoperative stress. Don’t be shy about discussing these feelings with your plastic surgeon.
The Procedure
Types of Breast Reconstruction
Your breast reconstruction surgery can be achieved through a variety of different techniques. The appropriate reconstructive procedure for you will be determined based on discussions with your surgeon, your body type, and prior therapy and/or surgical treatment.
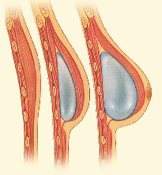
Implant Reconstructions
• Expander/Implant
First, a temporary device known as a tissue expander is placed in the breast to create the soft pocket that will contain the permanent implant. Some surgeons may also use an acellular dermal matrix to assist with reconstruction. Once expansion is complete, the expander will be exchanged for the permanent implant during an outpatient procedure. In expander/implant reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay (Mastectomy/Expander): 1 – 2 days
Recovery Time (Mastectomy/Expander): 4 – 6 weeks
Hospital Stay (Implant Exchange): Outpatient
Recovery Time (Implant Exchange): 1 – 2 weeks
• Direct-to-Implant
This approach allows for a breast implant to be placed immediately following mastectomy, foregoing the need for a tissue expander. Some patients may still require a secondary procedure. In direct-toimplant reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 1 – 2 days
Recovery Time: 4 – 6 weeks
Flap Reconstructions
• Donor Site: Abdomen
TRAM flap: The most common method of tissue reconstruction is the pedicled transverse rectus abdominus myocutaneous (TRAM) flap. In this approach, abdominal muscle, tissue, skin, and fat are used to create breast shape. The patient will have the benefit of a flatter looking abdomen. The scar on the abdomen is low and extends from hip to hip. In TRAM flap reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 2 – 5 days
Recovery Time: Several weeks to several months
• Donor Site: Abdomen
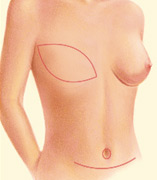
Breast Rectonstruction TRAM Flap
.jpg)
Abdominal free flap: These microsurgical (DIEP, SIEP) procedures may or may not use the actual abdominal muscle, so they may allow for results with fewer donor site complications. However, they are lengthier procedures and have the potential for other complications. These procedures should only be performed by plastic surgeons who perform microsurgery regularly and in institutions with experience in monitoring these flaps. In free flap reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 3 – 5 days
Recovery Time: Several weeks to several months
• Donor Site: Back
LD flap: The latissimus dorsi (LD) flap is most commonly combined with an implant. At the time of breast reconstruction, the muscle flap, with or without attached skin, is removed from the back and implanted in the breast. This flap provides a source of soft tissue that can help create a more natural looking breast shape compared to an implant alone. The scar on the back can often be concealed under a bra strap. In LD flap reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 1 – 3 days
Recovery Time: Several weeks



• Donor Site: Buttock
GAP flap: The gluteal artery perforator (GAP) free flap uses skin and fat from the buttocks. This type of reconstruction is technically more difficult to perform than other procedures. Also, the tissue from the buttock is somewhat harder to shape into a breast. In GAP free flap reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 3 – 5 days
Recovery Time: Several weeks
• Donor Site: Thigh
Inner thigh free flap: This procedure uses skin, fat, and muscle from the inner portion of the upper thigh to reconstruct the breast. The tissue is dissected from the inner thigh and transplanted to the chest where it is reattached using microsurgery. The resulting thigh scar is generally well hidden. In thigh free flap reconstructions, patients can expect the following to occur with some exceptions:
Hospital Stay: 3 – 5 days
Recovery Time: Several weeks
Implant Choices
Your plastic surgeon will talk to you about your breast reconstruction options. There are a number of different options for implants that may be used during your breast reconstruction.
Saline implants are filled with sterile salt water. They can be filled with varying amounts of saline which can affect the shape, firmness and feel of the breast. Should the implant shell leak, a saline implant will collapse and the saline will be absorbed and naturally expelled by the body. Saline implants can feel or look wrinkler in thin patients.
Silicone implants are filled with an elastic gel. The gel feels and moves much like natural breast tissue. If the implant leaks, the gel may remain within the implant shell, or may escape into the breast implant pocket. A leaking implant filled with silicone gel may not collapse. If you choose these implants, you may need to visit your plastic surgeon regularly to make sure the implants are functioning properly. An ultrasound or MRI screening can assess the condition of breast implants.
Shape
Form stable implants mimic the natural shape of the breast and are shaped like a tear drop. They are thicker at the bottom and tapered towards the top. \
They are usually filled with a cohesive gel. If they rotate, they may lead to a strange appearance. It is also usually necessary to have a longer incision with these implants.
Round implants have a tendency to make reconstructed breasts appear fuller than form stable implants. They also often will make the breast project out further away from the body. New high-profile options can lead to even more projection, if that is a concern for you. Because they are the same shape all over, there is less concern about them rotating out of place.
Texture
Textured breast implants allow the scar tissue to stick to the implant, making them less likely to move around inside of the breast and get repositioned.
Smooth breast implants move around freely inside of the breast, which may give more natural movement. These implants also have an increased risk of rippling.
Your plastic surgeon will take into account your wishes and concerns and will choose the right breast reconstruction option for you.
Implant manufacturers occasionally introduce new styles and types of implants, so there may be additional options available. Whether you choose saline or silicone implants, it is important for you to monitor your breast implants and follow up with your plastic surgeon for appropriate checkups.
Risks and Safety
The decision to have breast reconstruction is extremely personal. You will have to decide if the benefits will achieve your goals and if the risks and potential complications are acceptable. You will be asked to sign consent forms to ensure that you fully understand the procedure and any risks and potential complications.
The risks include:
- Anesthesia risks
- Bleeding (hematoma)
- Flap surgery includes the risk of partial or complete loss of the flap and a loss of sensation at both the donor and reconstruction site
- Infection
- Breast asymmetry
- Breast contour and shape irregularities
- Changes in nipple or breast sensation, which may be temporary or permanent
- Poor wound healing
- Persistent pain
- Possibility of revision surgery
- The use of implants carries the risk of breast firmness (capsular contracture) and implant rupture
- Unfavorable scarring
- Fat transfer risks include cysts, infection, microcalcification, necrosis (death) of fat cells and the possibility that some of the transferred fat cells will leave the breast area.
These risks and others will be fully discussed prior to your consent.
It is important that you address all of your questions directly with your plastic surgeon.
Recovery After Surgery
.jpg)
Following your surgery, gauze or bandages will be applied to your incisions. An elastic bandage or support bra will minimize swelling and support the reconstructed breast. A small, thin tube may be temporarily placed under the skin to drain any excess blood or fluid. A pain pump may also be used to reduce the need for narcotics. You will be given specific instructions that may include how to care for your surgical site(s) following surgery, medications to apply or take orally to aid healing and reduce the risk of infection, specific concerns to look for at the surgical site or in your general health, and when to follow up with your plastic surgeon.
Be sure to ask your plastic surgeon specific questions about what you can expect during your individual recovery period.
- Where will I be taken after my surgery is complete?
- What medication will I be given or prescribed after surgery?
- Will I have dressings/bandages after surgery?
- When will they be removed?
- Are stitches removed? When?
- When can I resume normal activity and exercise?
- When do I return for follow-up care?
Results
.jpg)
The results of breast reconstruction will be long-lasting, provided that you maintain a stable weight and general fitness. As your body ages, it is natural to lose some firmness, but most of your improvement should be relatively permanent.
Although good results are expected from your procedure, there is no guarantee. In some situations, it may not be possible to achieve optimal results with a single surgical procedure and another surgery may be necessary.
Over time, some breast sensation may return, and scar lines will improve, although they’ll never disappear completely. There are trade-offs, but most women feel these are small compared to the large improvement in their quality of life and the ability to look and feel whole. Careful monitoring of breast health through self-exam, mammography and other diagnostic techniques is essential to your long-term health.
Healing will continue for several weeks as swelling decreases and breast shape and position improve. Continue to follow your plastic surgeon’s instructions and attend follow-up visits as scheduled.
Cost
Prices for breast reconstruction can vary. A surgeon’s cost may be based on his or her experience, the type of procedure used, and geographic office location.
Cost may include:
- Anesthesia fees
- Hospital or surgical facility costs
- Medical tests
- Post-surgery garments
- Prescriptions for medication
- Surgeon’s fee
Breast reconstruction surgery after breast cancer is considered a reconstructive procedure and should be covered by health insurance. However, your coverage may only provide a small part of the total fee.
